Psoriasis is a chronic autoimmune condition that causes the rapid buildup of skin cells, leading to scaly, dry, and itchy skin. While there is no cure, certain lifestyle changes, medications, and tracking triggers can help manage the symptoms.
Psoriasis Overview
How Psoriasis Affects the Skin:
- Cell Buildup: Psoriasis accelerates the skin cell production process. Normally, skin cells grow deep within the skin and rise to the surface over about a month before shedding. In psoriasis, this cycle speeds up, causing cells to accumulate on the surface within days.
- Inflammation and Redness: Inflammation and redness are common around the scales.
- Appearance of Scales: Psoriatic scales are typically whitish-silver and form thick, red patches. On darker skin tones, they can appear more purplish or dark brown with gray scales. Sometimes, these patches may crack and bleed.
The Psoriasis Process:
- Normal Skin Cell Cycle: Skin cells grow deep within the skin and rise to the surface over about a month, eventually shedding off.
- Psoriasis Skin Cell Cycle: The process speeds up, causing skin cells to rise in just a few days. This rapid production prevents cells from shedding properly, leading to a buildup on the skin’s surface.
Where Psoriasis Usually Starts
Psoriasis scales commonly develop on joints, such as elbows and knees, but they can also appear on various other parts of the body. Here are the typical and less common areas affected by psoriasis:
What are the Different Types of Psoriasis?
There are five primary types of psoriasis, each with distinct characteristics:
Plaque Psoriasis
- This is the most common type, affecting about 80–90% of people with psoriasis, according to the American Academy of Dermatology (AAD).
- It causes red, inflamed patches on light skin tones and purple or grayish patches on darker skin tones, making it harder to diagnose in people of color.
- These patches are often covered with whitish-silver scales or plaques and are commonly found on the elbows, knees, and scalp.
Guttate Psoriasis
- Guttate psoriasis typically occurs in childhood.
- It causes small pink or violet spots, primarily on the torso, arms, and legs.
- These spots are rarely thick or raised like those in plaque psoriasis.
Pustular Psoriasis
- This type is more common in adults.
- It causes white, pus-filled blisters and broad areas of red or violet inflamed skin, with a more intense violet color on darker skin tones.
- Pustular psoriasis is usually localized to smaller areas such as the hands or feet but can also be widespread.
Inverse Psoriasis
- Inverse psoriasis leads to bright areas of red, shiny, inflamed skin.
- It typically develops under the armpits or breasts, in the groin, or around skin folds in the genital area.
Erythrodermic Psoriasis
- This is a severe and rare form of psoriasis, as noted by the National Psoriasis Foundation.
- It often covers large sections of the body, making the skin appear sunburned.
- Scales develop and may slough off in large sections or sheets.
- This type can be life-threatening, often accompanied by fever or severe illness, and requires immediate medical attention.

Common Areas:
- Elbows
- Knees
- Scalp
- Hands
- Feet
- Neck
- Face
Less Common Areas:
- Nails
- Mouth
- Area around the genitals
Associated Conditions:
Psoriasis is often linked with several other health conditions, including:
- Type 2 diabetes
- Inflammatory bowel disease
- Heart disease
- Psoriatic arthritis
- Anxiety
- Depression
Understanding where psoriasis typically manifests and its associated conditions can help in early detection and comprehensive management of the disease.
Symptoms:
- Scaly, dry, or itchy skin
- Inflammation and redness around the scales
- Whitish-silver or gray scales on thick, red or purplish patches
- Cracked and bleeding patches
Diagnosing Psoriasis
To diagnose psoriasis, two primary methods may be used:
- Physical Examination
- Most doctors can diagnose psoriasis through a simple physical exam. The symptoms of psoriasis are usually distinct and easily distinguishable from other conditions with similar symptoms.
- During the exam, it’s essential to show your doctor all areas of concern and mention if any family members have the condition.
2. Biopsy
- If the symptoms are unclear or if the doctor wants to confirm the diagnosis, they may take a small sample of your skin, known as a biopsy.
- Biopsies are typically done in the doctor’s office during the appointment. A local numbing medication is usually injected to minimize pain.
- The skin sample is sent to a lab for analysis, where it is examined under a microscope. This examination helps diagnose the type of psoriasis and rule out other potential disorders or infections.
- Once the results are available, the doctor may schedule an appointment to discuss the findings and potential treatment options.
Underlying Causes and Triggers:
Psoriasis triggers vary from person to person and can influence the onset, recurrence, or worsening of symptoms. Identifying and managing your specific triggers is essential for controlling the condition.
- Psoriasis is believed to be triggered by an overactive immune system and various genetic and environmental factors.
- Inflammation within the body contributes to the external symptoms, such as itchy, red plaques.
- The exact cause remains unknown, but it involves a combination of immune system dysfunction and other factors.

By understanding the underlying mechanisms and potential triggers of psoriasis, individuals can better manage the condition through appropriate treatments and lifestyle adjustments.
Who Does Scalp Psoriasis Affect?
Scalp psoriasis can affect anyone, but certain factors may increase your likelihood of developing it. You may be more prone to scalp psoriasis if you:
- Drink alcohol
- Experience stress or depression
- Have obesity
- Smoke or use tobacco products
- Take your medications infrequently
- Have other autoimmune diseases
Understanding these risk factors can help in managing and potentially reducing the severity of scalp psoriasis.
Is Psoriasis Genetic?
Psoriasis, like curly hair and eye color, is influenced by genetics. Approximately 1 in 3 individuals with psoriasis has a relative with the disease. Additionally, up to 10% of the population carries genes that predispose them to psoriasis, but only 2% to 3% will develop the condition.
While you can’t change your genetics, you can manage factors that trigger psoriasis symptoms.
Psoriasis Treatment, Medicine, and Skincare Products
Psoriasis is a chronic autoimmune condition that can be managed with a variety of treatments, medications, and skincare products. The choice of treatment often depends on the severity and location of the psoriasis, as well as individual patient preferences and responses. Here’s a breakdown of common options:
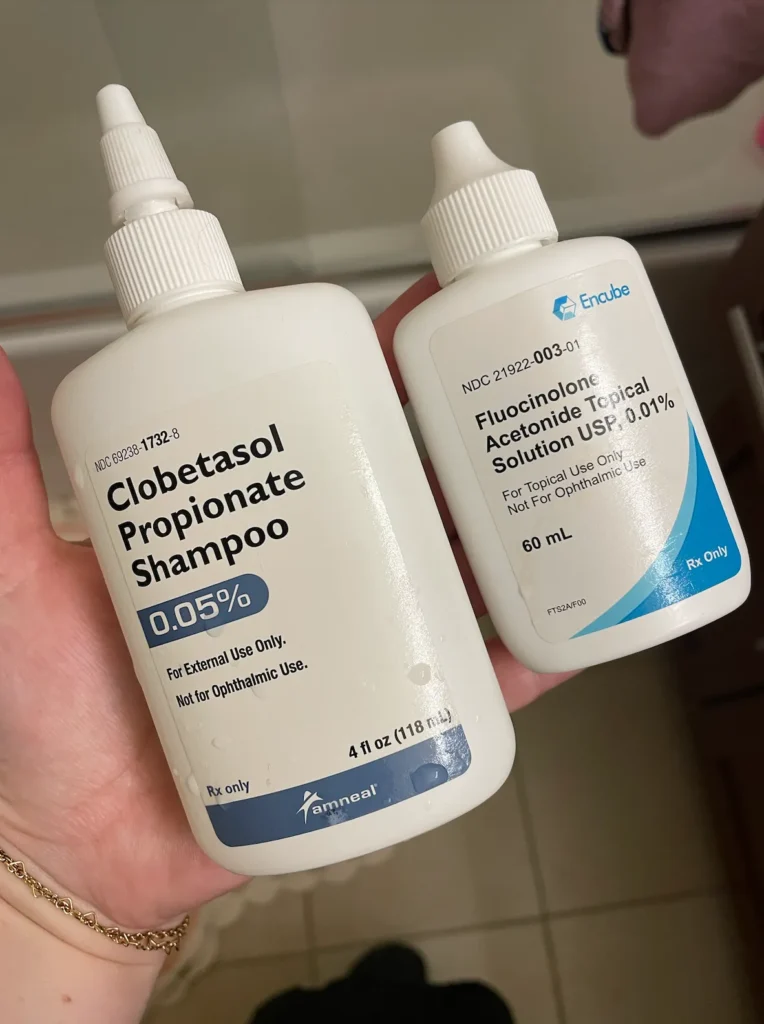
Topical Treatments
- Corticosteroids: Reduce inflammation and relieve itching. Available in various strengths, from mild to potent.
- Vitamin D Analogues: Slow skin cell growth. Examples include calcipotriene (Dovonex) and calcitriol (Vectical).
- Retinoids: Normalize skin cell growth. Tazarotene (Tazorac) is a common choice.
- Calcineurin Inhibitors: Reduce inflammation and plaque buildup. Examples are tacrolimus (Protopic) and pimecrolimus (Elidel).
- Salicylic Acid: Promotes shedding of dead skin cells to reduce scaling.
- Coal Tar: Reduces scaling, itching, and inflammation. Available in shampoos, creams, and oils.
Systemic Medications
- Methotrexate: Suppresses the immune system to reduce skin cell production.
- Cyclosporine: Another immunosuppressant used for severe cases.
- Acitretin: An oral retinoid that helps normalize skin cell growth.
- Biologics: Target specific parts of the immune system. Examples include adalimumab (Humira), etanercept (Enbrel), and ustekinumab (Stelara).
Light Therapy (Phototherapy)
- UVB Therapy: Uses ultraviolet B light to slow skin cell turnover.
- PUVA Therapy: Combines a drug called psoralen with UVA light to enhance effectiveness.
- Excimer Laser: Targets specific areas with high doses of UVB light.
Skincare Products
- Moisturizers: Essential for keeping the skin hydrated and reducing scaling. Look for heavy, fragrance-free options like Eucerin or Cetaphil.
- Medicated Shampoos: Often containing coal tar or salicylic acid for scalp psoriasis.
- Bath Solutions: Oatmeal baths or Epsom salts can soothe irritated skin.
- Barrier Creams: Products containing ingredients like petrolatum or zinc oxide to protect and heal the skin.
Lifestyle Changes
- Diet and Nutrition: A balanced diet rich in anti-inflammatory foods can help manage symptoms.
- Stress Management: Techniques such as meditation, yoga, or counseling can reduce flare-ups triggered by stress.
- Regular Exercise: Helps improve overall health and reduce stress.
Alternative Therapies
- Aromatherapy: Essential oils like lavender or chamomile can help reduce stress and promote skin healing.
- Acupuncture: May improve blood circulation and reduce symptoms for some people.
Conclusion
Managing psoriasis often requires a combination of treatments tailored to individual needs. Consulting with a dermatologist is crucial for developing a comprehensive treatment plan that effectively addresses your specific condition.
